Finally, we’re in a position to release the results of the study. All seven feasibility objectives have been analysed, together with a look at the average difference in symptoms and quality of life scores between baseline and three-month follow-up. You can download the PDF here, or if you prefer, you can read it on this page.
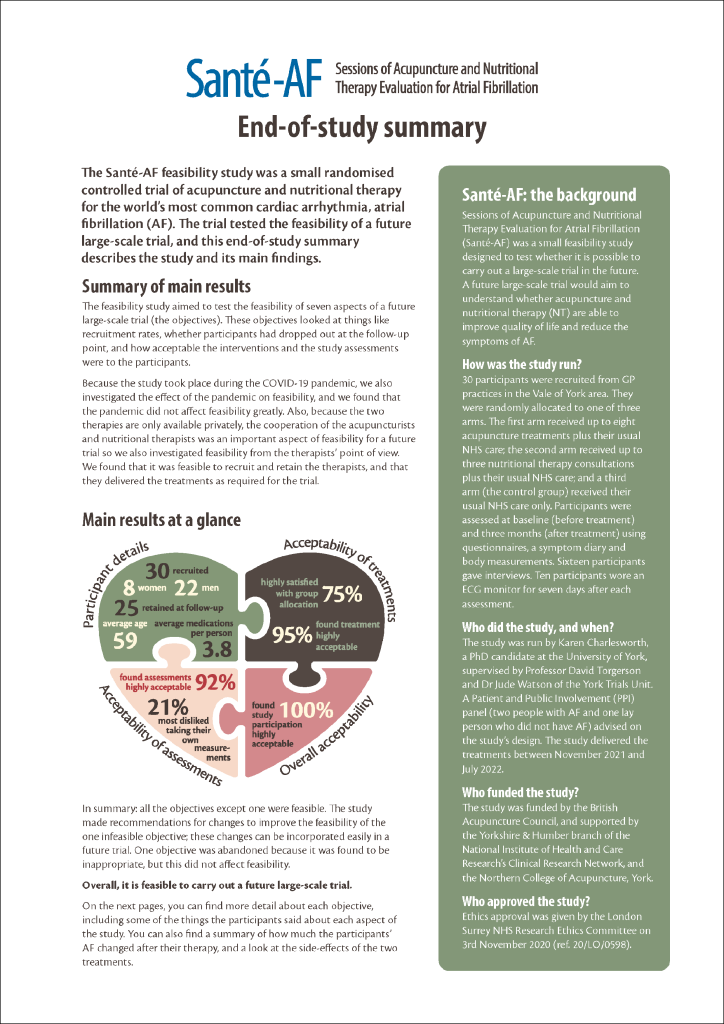
Summary of the main results: The feasibility study aimed to test the feasibility of seven aspects of a future large-scale trial (the objectives). These objectives looked at things like recruitment rates, whether participants had dropped out at the follow-up point, and how acceptable the interventions and the study assessments were to the participants.
Because the study took place during the COVID-19 pandemic, we also investigated the effect of the pandemic on feasibility, and we found that the pandemic did not affect feasibility greatly. Also, because the two therapies are only available privately, the cooperation of the acupuncturists and nutritional therapists was an important aspect of feasibility for a future trial so we also investigated feasibility from the therapists’ point of view. We found that it was feasible to recruit and retain the therapists, and that they delivered the treatments as required for the trial.
In summary: all the objectives except one were feasible, and overall it is feasible to carry out a large-scale trial using the broad design of this feasibility study. The study made recommendations for changes to improve the feasibility of the one infeasible objective; these changes can be incorporated easily in a future trial. One objective was abandoned because it was found to be inappropriate, but this did not affect feasibility.
Objective 1: Were participants willing to take part?
FEASIBLE. We answered this question in several different ways. First, we looked at the number of people who were enrolled in the trial, compared with the number who were actually eligible to take part. We found that 96.8% of people who were eligible went on to be enrolled. The threshold for feasibility was to enrol 90% or more of people who were eligible, so this objective was judged to be feasible in a future trial without needing any changes.
We also looked at the things that people said about why they wanted or didn’t want to take part. When asked which was the most important reason in wanting to take part, people singled out curiosity about acupuncture (21%) and wanting to help others with AF (21%). The most frequent reasons for not wanting to take part were not having internet or computer skills (3 people) and not willing to have acupuncture (2 people). Four people felt they could not give the time needed. Of course not every potential participant got in touch to tell us why they didn’t want to take part, so this part of our analysis can’t be certain.
Finally, we looked at whether people’s preferences for and against acupuncture or nutritional therapy affected willingness to take part, and found that preferences had very little effect.
Objective 2: Were the eligibility criteria appropriate?
NOT FEASIBLE. The study’s eligibility criteria were not feasible for a future trial because they excluded a large number of people (93% of the people identified by the GP practices), meaning that a future trial using these criteria may not be able to recruit enough participants. In addition, the exclusions meant that the study’s participants may not have been representative of people with AF in general, and this would mean that a future trial’s results may not have applied to other people with AF. The elibility criterion that affected the greatest number of people was the age range (45–70) – this excluded 74% of the people identified by GP practices.
The study recommended changes to the eligibility criteria for a future trial. These included removing the age restriction, removing the restrictions on the type of AF and its severity, and removing the COVID-19 vulnerability criteria (unless a future trial happened under pandemic conditions). These changes are easy to incorporate in a future trial; they would increase the likelihood of the trial being able to recruit enough people, and they would make it more representative of a general population of people with AF.
Objective 3: Did the participants stay in the study or did they drop out?
FEASIBLE. Of the 30 people recruited, five dropped out (three in the Nutritional Therapy arm, and two in the Usual Care arm). All people in the Acupuncture arm stayed in the study. The threshold for feasibility was set at 80% of people staying in the study; 83% of the participants stayed, so this objective was judged to be feasible without changes.
We analysed the reasons why the five people left the study. One left due to illness; another had unexpected caring responsibilities and wasn’t able to complete the follow-up assessment. Two didn’t give a reason for dropping out, and one dropped out because they were randomly allocated to the Usual Care group and were disappointed that they wouldn’t be having either acupuncture or nutritional therapy. People stayed for a range of reasons, including “not being a quitter” and doing the study “for the general good”.
The study made some recommendations to increase the number of people who would remain in a future trial. These included making sure the therapists’ premises were closer to participants’ homes; and offering people in the Nutritional Therapy group a choice about whether their appointments were online or in person.
Objective 4: Were the two therapies acceptable to participants?
FEASIBLE. People who were randomly allocated to the Acupuncture or Nutritional Therapy arms found the two therapies highly acceptable (95% of people in the treatment arms). This objective had a feasibility threshold of 75% or more of participants finding their treatments acceptable, so it was judged to be feasible without changes. Attendance across both therapies was high, at 92%. People gave various reasons for finding the therapies acceptable, including the positive effects of the treatments and enjoying the relationship with the practitioner. Downsides of the two therapies included travelling time and stress in the Acupuncture arm; and in the Nutritional Therapy arm, one person discussed the costs and effort involved in making dietary changes, especially when cooking for a household.
The study recommended changes to increase the therapies’ acceptability further, including making sure that therapists’ premises are closer to participants’ homes, and making sure that nutritional therapists adjust diet plans to consider the needs of households.
Objective 5: Were the study assessments acceptable to participants?

FEASIBLE. All participants did an assessment twice during the study. Each assessment involved people filling in a questionnaire, taking measurements of their waist and hips, weighing themselves, taking a blood pressure reading, and giving details of medications. Sixteen people took part in interviews in addition, and 10 people were guided to fit themselves with a seven-day CardioSTAT® ECG monitor. The assessments were done online to minimise the risk of COVID-19 infection.
The assessments were found to be highly acceptable by 92% of participants. The feasibility threshold for this objective was 90% or more finding the assessments highly acceptable, so this objective was feasible without the need for changes. We thought there might have been a link between the length of an assessment and its acceptability (in other words, the longer the assessment, the less acceptable it was), but this was not true: in fact, some people doing the longest assessments found them to be the most acceptable.
But participants did find the assessments difficult in various ways, including disliking taking their own measurements (21%), and disliking the online format (16%); the follow-up questionnaire was particularly disliked (20%). The study recommended some changes to reduce these difficulties, including holding assessments in person at a study centre where participants could be weighed and have their measurements taken by a healthcare professional, and reducing the length of questionnaires.
Objective 6: Was the CardioSTAT® heart monitor useful to the study?

ABANDONED. The CardioSTAT® ECG monitor was a small device that 10 people in the study fitted to their own chest to measure their symptoms over a seven-day period. We looked at whether participants’ symptom diaries were similar to the ECG monitor readings – in other words, when these 10 people felt their AF, was it actually AF according to the monitor? We found that there was very little similarity between the two. Sometimes people had AF but didn’t record it in the diary (perhaps because they weren’t feeling it); and we also found the opposite, where people felt AF although no AF was actually happening. This was a useful finding for a future trial because it showed that people’s perceptions of AF are not necessarily accurate. So in a future trial there are good reasons to use the monitor, to get a more objective reading of actual symptoms. We also found it was important to ask people to keep a symptom diary in a future trial, because in this study they were clearly experiencing something that could affect their quality of life (whether it was actual AF or not) – so in a future trial it will be important to record people’s own perceptions as well as actual AF.
We also asked people about their experience of fitting the monitor, wearing it, and returning it. They said it was generally easy to fit, comfortable to wear, and easy to return. This means a future trial should not have difficulty in asking people to use the monitor. However, most people were not very confident that the monitor was working well and detecting their symptoms. This may be because people had self-fitted the monitor, rather than a healthcare professional fitting it for them. Finally, we asked people whether the monitor had been an incentive to take part in the study. Three people said it was the most important reason to take part; only one person said it was their most important reason for staying in the study.
Although these findings are very useful for a future trial, none of them affected feasibility. The study originally set two feasibility thresholds for this objective, but during analysis it became clear that setting thresholds for the monitor’s usefulness wasn’t appropriate. So this objective became exploratory, and no feasibility threshold was applied.
Objective 7: How did participants find the overall experience of study participation?
FEASIBLE. We asked participants how they had found the overall experience of participating in the study. We found that 100% of participants thought it was acceptable, with 84% finding it extremely or very acceptable (the highest two ratings).
We also asked participants about the parts of the study they had most disliked. The two most disliked aspects were reading the participant information pack (17% felt this was too long, and gave too much information that wasn’t necessary), and hearing about their group placement (17% had a preference to be in another arm of the study, and were disappointed not to be in that arm). The study recommended changes to reduce the length of the participant information pack. However, we did not make a recommendation that participants should be given the treatment of their preference in a future trial. This is because preferences, although evident and sometimes strong, didn’t affect the overall feasibility of the study; and because allowing preferences would introduce bias in the results of a future trial, meaning the results would not be reliable.
Were acupuncture and nutritional therapy effective for AF symptoms and quality of life?
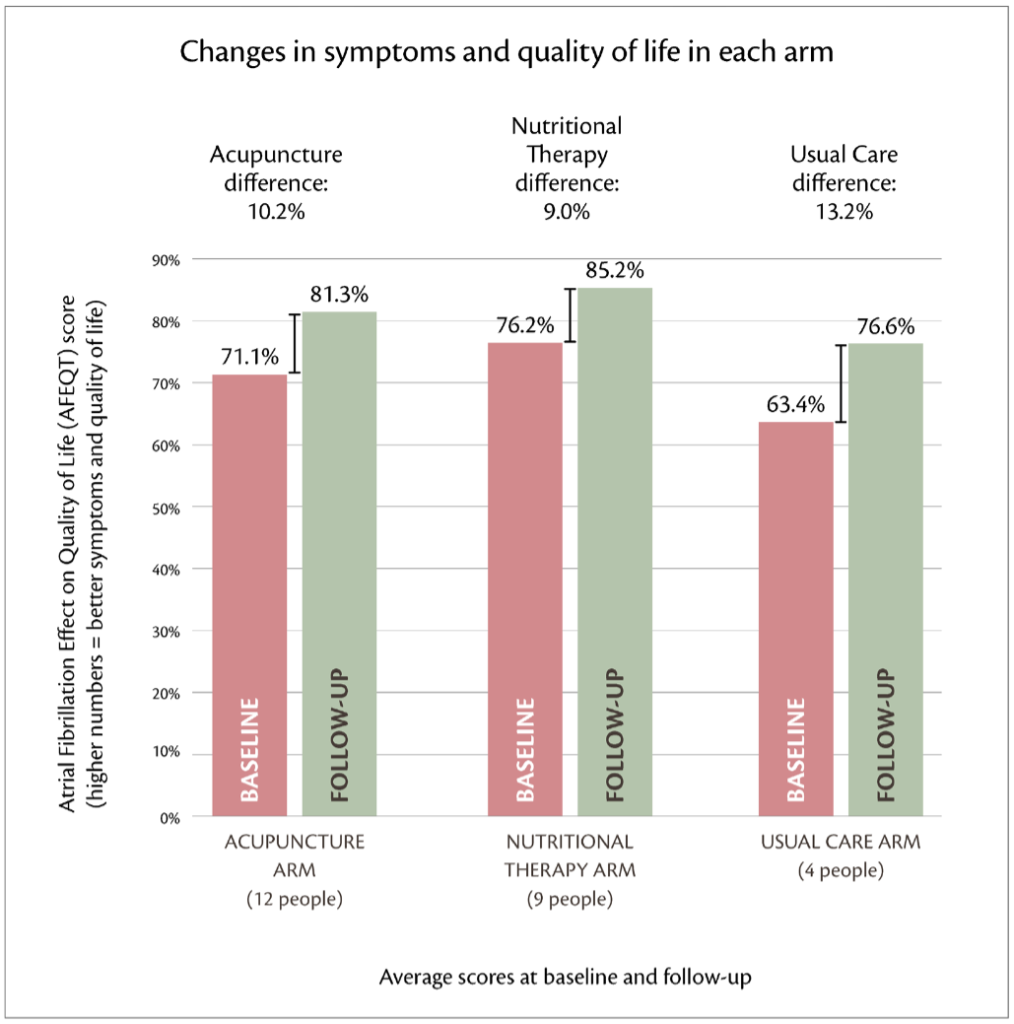
Because only 30 people took part in the Santé-AF feasibility study, there weren’t enough people to show whether acupuncture and nutritional therapy were effective or not. A future large-scale trial will be able to answer this question fully. But the feasibility study did explore the amount of change experienced by the participants for both symptoms and quality of life, and the results of this can be seen in the diagram on the right. We used a scale called the Atrial Fibrillation Effect on Quality of Life (AFEQT). We calculated the amount of change in each group by measuring participants once at baseline (before treatment) and a follow-up point at three months (after treatment) and comparing the two measurements, then averaging these “change scores” across each group.
Previous research has found that a “clinically important difference” for the AFEQT scale is 5.4 points (5.4%). In other words, people who experience an improvement of 5.4% on the AFEQT scale should notice an improvement in their AF symptoms and quality of life. The diagram shows that the two treatment groups in Santé-AF both experienced an improvement of around double this amount. This means that both treatments show promise.
What the diagram also shows is that the people in the Usual Care group (who didn’t have acupuncture or nutritional therapy) also improved; in fact, they improved more than the people in the Acupuncture or Nutritional Therapy groups. This is mainly because there were only four people remaining in the Usual Care group at the follow-up measurement point and most of them happened to record unusually large changes that skew the results. With more people in the group, which would happen in a large-scale trial, these measurements are likely to average out.
Were acupuncture and nutritional therapy safe?
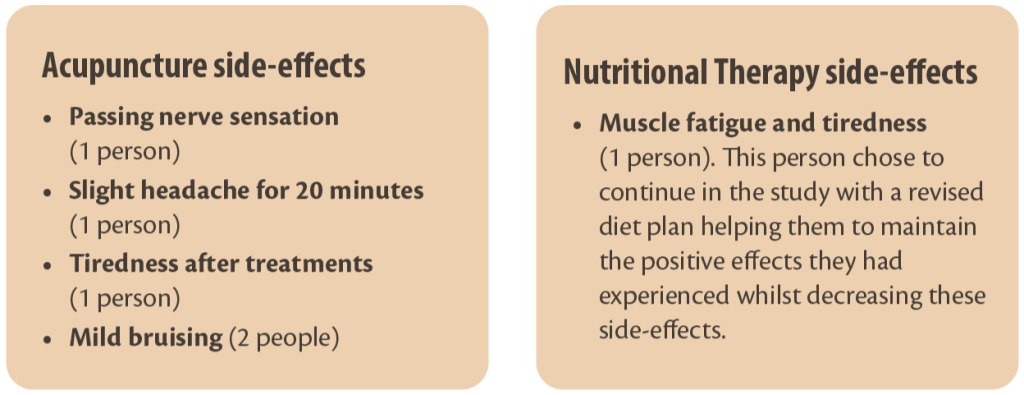
In the feasibility study, we looked at the safety of the two treatments (again with the caveat that 30 people isn’t enough to properly answer the question). We found that five people in the Acupuncture group experienced a range of mildly adverse side-effects, and one person in the Nutritional Therapy group experienced a moderately adverse side-effect. This compares well with the side-effects and safety of conventional medicine for AF.
Final conclusion
The Santé-AF feasibility study found that it is feasible to carry out a future large-scale trial. Feasibility can also be improved by changing the eligibility criteria, moving assessments to a study centre rather than online, and shortening the assessments. These adjustments would also improve the applicability of a future trial’s results to the general population of people with AF.
The study has helped patients by opening an investigation into different treatments for AF that may help to decrease symptoms and increase quality of life without the risks and side-effects of conventional medical treatments. The study also helped researchers by decreasing the uncertainty of a future large-scale trial, making it more efficient to conduct, and making its results more applicable to the general AF population.
If you have any questions about Santé-AF, please use our contact form to get in touch. Thanks for reading about the trial and sharing the journey!